Septal Infarct: What It Is, How It Happens, and How It Affects Your Heart
What is a septal infarct?
A septal infarct is a type of heart attack that damages the septum, which is the muscular wall that separates the right and left ventricles of the heart. The ventricles are the lower chambers of the heart that pump blood to the lungs and the rest of the body. The septum helps to maintain the proper pressure and flow of blood in each ventricle.
A septal infarct occurs when one or more of the coronary arteries that supply blood to the heart muscle become blocked by a blood clot or plaque, a fatty substance that builds up in the artery walls. This reduces or stops the blood flow to the part of the septum that is served by the affected artery, causing the tissue to die or become scarred. This can impair the function and structure of the heart, leading to serious complications such as heart failure, arrhythmia, or cardiac arrest.
How common is a septal infarct?
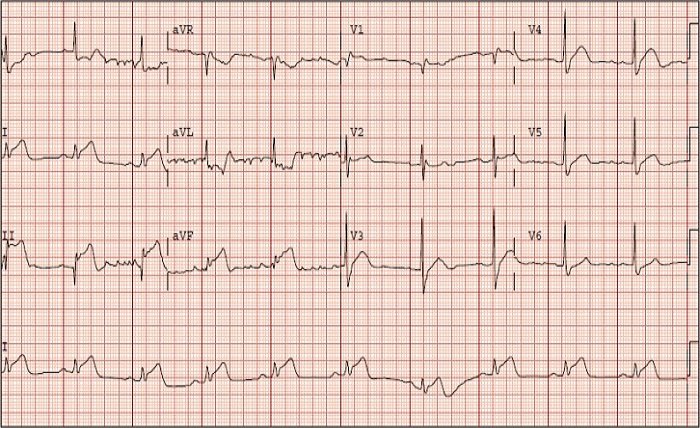
A septal infarct is not a very common type of heart attack, accounting for about 1% to 7% of all cases. However, it can be difficult to diagnose because it may not cause typical symptoms such as chest pain or shortness of breath. Some people may have a silent septal infarct, which means they have no symptoms at all or they are not recognized as signs of a heart attack. A silent septal infarct may only be detected by an electrocardiogram (ECG), a test that measures the electrical activity of the heart.
A septal infarct can affect anyone, but some factors may increase the risk, such as:
- Age: The risk of a septal infarct increases with age, especially after 65 years.
- Sex: Men are more likely to have a septal infarct than women, although the gap narrows after menopause.
- Family history: Having a close relative who had a septal infarct or another type of heart attack may increase the risk.
- Smoking: Smoking damages the blood vessels and increases the chance of developing plaque and blood clots.
- High blood pressure: High blood pressure puts extra strain on the heart and damages the arteries.
- High cholesterol: High cholesterol levels can contribute to plaque formation in the arteries.
- Diabetes: Diabetes affects the blood sugar levels and can damage the nerves and blood vessels.
- Obesity: Obesity increases the workload of the heart and raises the risk of other conditions that can lead to a septal infarct.
- Sedentary lifestyle: Lack of physical activity can weaken the heart muscle and increase the risk of other diseases that can affect the heart.
- Stress: Stress can trigger hormonal changes that can affect the blood pressure and heart rate.
How is a septal infarct diagnosed and treated?
A septal infarct can be diagnosed by various tests, such as:
- Electrocardiogram (ECG): An ECG records the electrical signals of the heart and can show if there is any damage or abnormality in the heart muscle. A septal infarct may cause specific changes in the ECG pattern, such as Q waves or ST segment elevation in certain leads.
- Echocardiogram: An echocardiogram uses sound waves to create an image of the heart and can show how well it is pumping and if there is any damage or enlargement in the septum or other parts of the heart.
- Cardiac catheterization: A cardiac catheterization involves inserting a thin tube called a catheter into an artery in the groin or arm and guiding it to the heart. A dye is injected through the catheter and an X-ray is taken to see if there are any blockages or narrowing in the coronary arteries.
- Magnetic resonance imaging (MRI): An MRI uses a strong magnetic field and radio waves to create detailed images of the heart and can show if there is any scar tissue or inflammation in the septum or other parts of the heart.
Read more about: remakerai.in
A septal infarct can be treated by various methods, depending on its severity and location. Some of these methods are:
- Medications: Medications can help to relieve pain, reduce inflammation, dissolve blood clots, lower blood pressure, control cholesterol levels, prevent arrhythmia, and improve blood flow to the heart. Some examples are aspirin, nitroglycerin, heparin, beta blockers, statins, calcium channel blockers, and antiarrhythmics.
- Angioplasty: Angioplasty is a procedure that involves inserting a catheter with a balloon at its tip into an artery in the groin or arm and guiding it to the blocked coronary artery. The balloon is then inflated to widen the artery and restore blood flow. A stent, a small metal mesh tube, may also be placed in the artery to keep it open.
- Coronary artery bypass graft (CABG): CABG is a surgery that involves taking a healthy blood vessel from another part of the body, such as the chest, leg, or arm, and attaching it to the heart to bypass the blocked coronary artery and create a new route for blood flow.
- Septal repair: Septal repair is a surgery that involves repairing or replacing the damaged part of the septum with a patch or a prosthetic device. This can help to restore the normal function and structure of the heart.
Read more about: facecheckid.in
What are the complications and prognosis of a septal infarct?
A septal infarct can cause various complications, such as:
- Heart failure: Heart failure is a condition in which the heart cannot pump enough blood to meet the body’s needs. This can cause symptoms such as fatigue, shortness of breath, swelling in the legs or abdomen, and reduced exercise capacity.
- Arrhythmia: Arrhythmia is a condition in which the heart beats too fast, too slow, or irregularly. This can cause symptoms such as palpitations, dizziness, fainting, chest pain, and difficulty breathing. Some types of arrhythmia can be life-threatening, such as ventricular fibrillation, which causes the heart to quiver instead of pumping blood.
- Cardiac arrest: Cardiac arrest is a condition in which the heart stops beating suddenly and unexpectedly. This can cause loss of consciousness, no pulse, no breathing, and death within minutes if not treated promptly.
- Septal rupture: Septal rupture is a rare but serious complication in which the damaged part of the septum tears or breaks open. This can cause blood to leak from one ventricle to another, creating a hole or a shunt. This can lead to severe heart failure, shock, and death.
The prognosis of a septal infarct depends on several factors, such as:
- The size and location of the infarct
- The extent and duration of the ischemia (lack of blood flow)
- The presence and severity of other heart conditions
- The age and overall health of the patient
- The timeliness and effectiveness of the treatment
Read more about: downloadhub4u
conclusion
The mortality rate of a septal infarct is higher than that of other types of heart attacks, ranging from 10% to 40%. However, with prompt diagnosis and treatment, many people can survive and recover from a septal infarct. The long-term outlook depends on how well the patient follows their doctor’s advice on medications, lifestyle changes, and follow-up care.
Read more about: guiterly